Your Ultimate Guide to Polycystic Ovary Syndrome (PCOS)
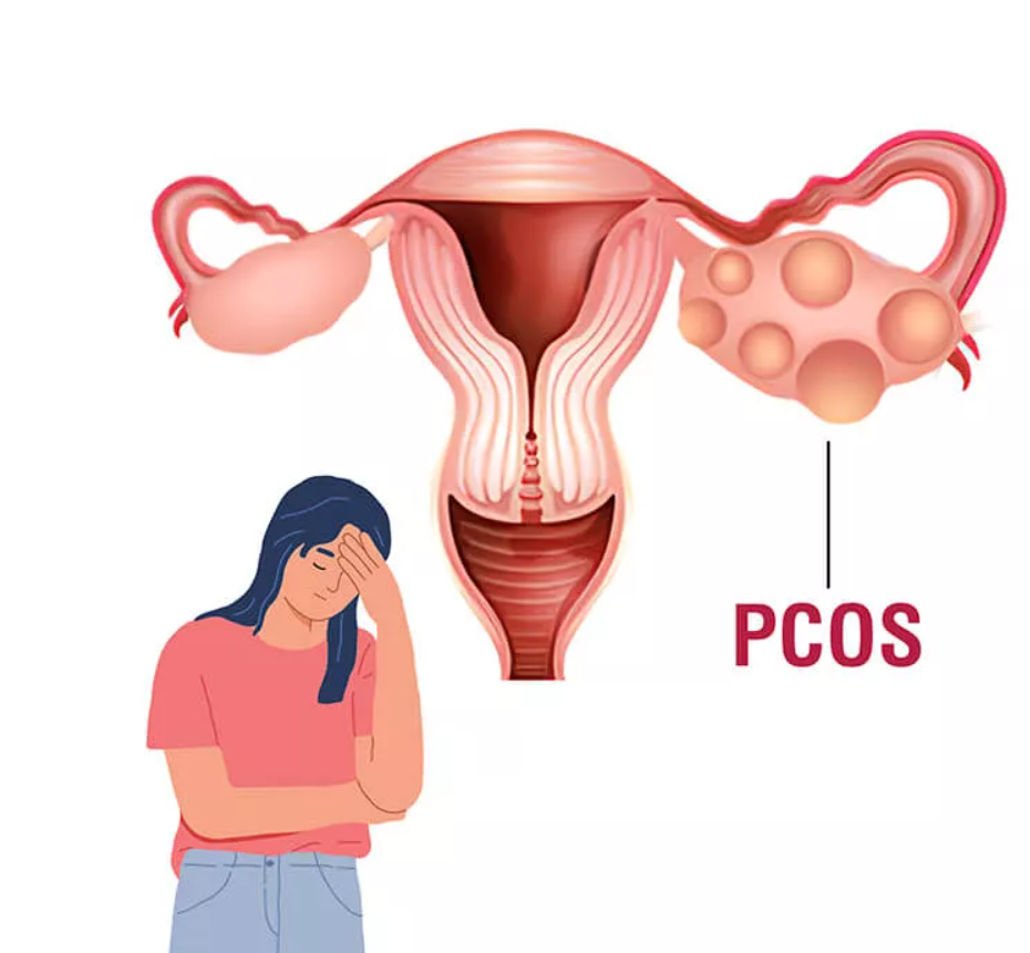
Polycystic Ovary Syndrome (PCOS) is a prevalent yet often misunderstood hormonal disorder that affects many individuals with ovaries. This comprehensive guide covers everything you need to know about PCOS, including its types, symptoms, causes, risk factors, and treatment options.
What Is PCOS?
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder characterized by an imbalance in sex hormones. This condition impacts how ovaries function, leading to irregular menstrual cycles, elevated androgen levels, and cysts on the ovaries. It affects approximately 6-12% of individuals of childbearing age and can have significant implications for reproductive and overall health.
Types of PCOS
Polycystic Ovary Syndrome (PCOS) can manifest in several forms, each with its unique features:
Classic PCOS: The most common type, characterized by irregular menstrual cycles, high levels of androgens (male hormones), and ovarian cysts.
Adrenal PCOS: Results from excess androgen production by the adrenal glands, which can cause symptoms similar to classic PCOS but is driven by adrenal imbalances.
Inflammatory PCOS: Associated with chronic inflammation, this type involves heightened inflammatory markers and can worsen overall symptoms.
Insulin-Resistant PCOS: Linked to insulin resistance and often accompanied by obesity, this type involves high insulin levels that exacerbate hormonal imbalances.
PCOS and Hormones
Hormonal imbalances are central to PCOS:
Androgens: Elevated levels of androgens such as testosterone leads to symptoms like excessive hair growth and acne.
Insulin: Many with PCOS experience insulin resistance, which can cause high blood sugar levels and increase the risk of type 2 diabetes.
Estrogen and Progesterone: Imbalances in these female hormones can result in irregular menstrual cycles and problems with ovulation.

PCOS Symptoms
Polycystic Ovary Syndrome (PCOS) symptoms can differ from person to person, but typically include:
Irregular Menstrual Cycles: Infrequent, irregular, or prolonged periods.
Excessive Hair Growth: Especially in areas like the face, chest, and back.
Acne and Oily Skin: Resulting from elevated androgen levels.
Thinning Hair: Hair loss on the scalp or thinning hair.
Weight Gain: Often associated with insulin resistance.
Dark Skin Patches: Known as acanthosis nigricans, typically found on the neck, armpits, or groin.
PCOS Causes
The precise cause of PCOS is not fully understood, but several factors may contribute:
Genetics: Family history of PCOS or similar conditions can increase risk.
Insulin Resistance: Many individuals with PCOS have insulin resistance, which can contribute to higher blood sugar levels.
Inflammation: Chronic low-grade inflammation may exacerbate PCOS symptoms.
Hormonal Imbalances: Disruptions in androgens and estrogens are central to the condition.
PCOS Risk Factors
Several factors can elevate the risk of developing PCOS:
Family History: A genetic predisposition may make you more susceptible.
Obesity: Excess weight is linked with insulin resistance and can worsen PCOS symptoms.
Type 2 Diabetes: Increased risk due to insulin resistance and metabolic issues.
What Are the Complications of PCOS?
If left unmanaged, Polycystic Ovary Syndrome (PCOS) can lead to several complications:
Infertility: Irregular ovulation can pose challenges to becoming pregnant.
Type 2 Diabetes: Increased risk due to insulin resistance.
Heart Disease: Higher risk of cardiovascular problems.
Endometrial Cancer: Prolonged exposure to estrogen without regular menstruation can increase risk.
Sleep Apnea: More common in individuals with obesity and insulin resistance.
PCOS Diagnosis
Diagnosing Polycystic Ovary Syndrome (PCOS) typically involves:
Medical History: Reviewing menstrual cycles, symptoms, and family history.
Physical Examination: Checking for symptoms such as excessive hair growth and acne.
Ultrasound: To detect cysts on the ovaries.
Blood Tests: Measuring hormone levels and assessing insulin resistance.
PCOS Treatment
Treatment for Polycystic Ovary Syndrome (PCOS) is personalized and may include:
Medications: Birth control pills to regulate menstrual cycles, anti-androgens to manage hair growth and acne, and insulin-sensitizing agents like metformin.
Lifestyle Changes: Adopting a balanced diet and regular exercise to manage weight and improve insulin sensitivity.
Ovulation Induction: For those trying to conceive, medications like clomiphene citrate or letrozole can help stimulate ovulation.
PCOS and Pregnancy
If you have Polycystic Ovary Syndrome (PCOS) and are attempting to conceive, consult a healthcare provider if:
You’ve been attempting to get pregnant for more than a year without success.
You experience severe menstrual irregularities or an absence of periods.
You have other symptoms, such as significant weight gain or high blood pressure, that might affect pregnancy.
Adjustments in Diet and Lifestyle for Managing PCOS and Enhancing Fertility
Effective management of Polycystic Ovary Syndrome (PCOS) often involves:
Balanced Diet: Emphasize the inclusion of whole grains, lean proteins, fruits, and vegetables in your diet.
Regular Exercise: Helps with weight management and improves insulin sensitivity.
Weight Management: Even modest weight loss can improve symptoms and increase fertility.
Alternative Medicine for PCOS
Some individuals explore alternative treatments, including:
Herbal Supplements: Spearmint tea, saw palmetto, and inositol may provide symptom relief.
Acupuncture: May support hormonal balance and ovulation.
Yoga and Stress Management: Techniques to reduce stress and promote overall well-being.
PCOS and Menopause
As individuals with Polycystic Ovary Syndrome (PCOS) approach menopause:
Symptoms May Persist: Issues like insulin resistance and weight gain may continue.
Hormonal Changes: Menopause can alter PCOS symptoms and management strategies may need adjustment.
Takeaways
PCOS is a multifaceted condition that affects various aspects of health. Effective management includes a combination of lifestyle changes, medications, and sometimes alternative therapies. Early diagnosis and proactive treatment are key to managing symptoms and reducing the risk of complications.
If your symptoms are severe or don’t improve, don’t wait—schedule an appointment at Lux Hospital for expert care and treatment. We focus on your comfort and well-being first.
Frequently Asked Questions
PCOS cannot be cured, but its symptoms can be effectively managed with appropriate treatment and lifestyle adjustments.
Yes, PCOS often runs in families, indicating a genetic component.
PCOS can increase the risk of type 2 diabetes, heart disease, and endometrial cancer, making ongoing management and regular health check-ups important.