Stages of Chronic Kidney Disease: What You Need to Know
Chronic kidney disease (CKD) is a silent, progressive illness that affects millions of individuals globally. Your kidneys must eliminate waste and excess blood fluids, assisting in the regulation of electrolytes, blood pressure, and red blood cell formation. When they begin to fail, it doesn’t happen all at once it unfolds over several stages. By being aware of the five stages of chronic kidney disease (CKD), you may take control of your health and halt the illness’s progression.
This blog will describe the steps you may take to safeguard your kidney function, along with an explanation of each stage and what’s going on in your body.
What is Chronic Kidney Disease?
A gradual decrease in kidney function over time is called chronic kidney disease (CKD). Chronic illnesses are typically the cause:
- Diabetes
- High blood pressure
- Recurrent kidney infections
- Autoimmune diseases
- Polycystic kidney disease
CKD is diagnosed and monitored using a glomerular filtration rate (GFR) blood test. This test estimates how well the kidneys filter blood. The lower the GFR, the worse the kidney function.
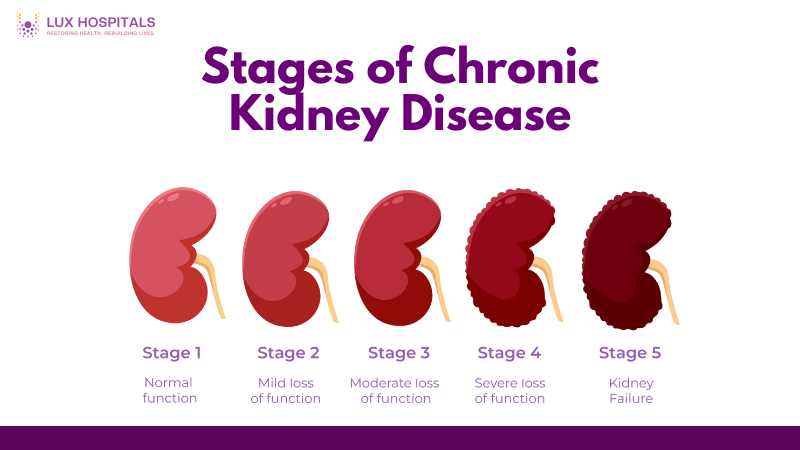
Stages Of Chronic Kidney Diseases
5 Stages of Chronic kidney disease (CKD), ranging from Stage 1 (minimal damage) to Stage 5 (total renal failure).
Stage 1: Damage to the kidneys with normal or high GFR
- GFR: ≥ 90 mL/min/1.73 m²
- Kidney Function: Normal
- Symptoms: Usually no symptoms
- Common Causes: High blood pressure, diabetes, family history of kidney disease
Although your kidneys are still healthy at Stage 1, there are indications of damage, such as proteinuria (protein in the urine) or abnormalities in imaging studies. At this point, most patients are not aware that they have kidney disease because the symptoms are either nonexistent or very mild.
What You Can Do:
- Control blood sugar and blood pressure.
- Avoid overuse of painkillers (NSAIDs)
- Stay hydrated
- Eat a balanced, kidney-friendly diet.
- Get regular checkups and kidney function tests.
Stage 2: Mild Reduction in Kidney Function
- GFR: 60–89 mL/min/1.73 m²
- Kidney Function: Mildly decreased
- Symptoms: Still typically asymptomatic, though some people may notice fatigue or swelling
Stage 2 indicates a slight loss in kidney function, but you might still feel good. Early identification and management of the root problem of kidney disease is crucial to halting its progression.
What You Can Do:
- Monitor and manage risk factors (especially diabetes and hypertension)
- Avoid smoking and excessive alcohol.
- Begin working with a healthcare provider or nephrologist , urologists.
- Consider dietary changes (reduced salt and protein intake)
Stage 3: Moderate Reduction in Kidney Function
- Stage 3a: GFR 45–59 mL/min
- Stage 3b: GFR 30–44 mL/min
- Symptoms: Fatigue, swelling (especially in the ankles and feet), changes in urination, back pain, anemia, or bone disease
Stage 3 is often when CKD becomes more noticeable. You may begin experiencing symptoms and complications such as electrolyte imbalances, fluid retention, and elevated blood pressure. Early management can significantly slow further damage.
What You Can Do:
- Work closely with a nephrologist or urologists.
- Manage complications like anemia, high phosphorus, and calcium imbalance.
- Follow a kidney-friendly diet (lower protein, sodium, and phosphorus)
- Take prescribed medications consistently.
- Monitor lab values and adjust treatment as needed.
Stage 4: Severe Reduction in Kidney Function
- GFR: 15–29 mL/min/1.73 m²
- Kidney Function: Severely decreased
- Symptoms: More frequent and severe nausea, itching, poor appetite, difficulty concentrating, sleep disturbances, muscle cramps
In Stage 4, your kidneys are significantly impaired, and you’re likely experiencing a noticeable impact on your quality of life. This is a critical time to prepare for the possibility of kidney replacement therapy (dialysis or transplant).
What You Can Do:
- Prepare for dialysis or transplant, learn about options and make decisions early.
- Continue to manage contributing conditions.
- Follow a rigorous kidney-friendly diet (consult a renal dietitian)
- Check your fluid intake and electrolyte levels.
- Take proactive measures with your healthcare team to control your symptoms.
Stage 5: Kidney Failure (End-Stage Renal Disease)
- GFR: <15 mL/min/1.73 m² or on dialysis
- Kidney Function: Minimal to none
- Symptoms: Severe dyspnea, nausea, confusion focusing, edema, uremic frost (rare), and in severe situations, coma
This is the final stage of CKD, where The ability of kidneys to work independently has almost completely disappeared. If waste and fluid are not handled, they become dangerous. Most people in Stage 5 will need dialysis or a kidney transplant to survive.
Treatment Options For Stages of Chronic Kidney Diseases
- Hemodialysis: A dialysis machine is used in a clinic to filter blood. Using a catheter at home, waste is filtered through the abdominal lining during peritoneal dialysis.
- Kidney transplant: Normal function is restored with a new kidney from a donor.Symptom-focused, non-dialysis care is what conservative treatment some patients opt for.
Tips for Preventing CKD Progression
The following advice can help safeguard your kidney function, regardless of whether you have early-stage CKD or are at risk for it, or already in one of the stages of Chronic Kidney Disease.
- Monitor blood pressure and blood sugar regularly.
- Keep up your exercise routine and keep your weight in check.
- Avoid overuse of NSAIDs like ibuprofen and naproxen.
- Give up smoking since it lowers kidney blood flow.
- Stay hydrated, but avoid excess fluid if you’re in advanced stages.
- Get regular lab tests including GFR, creatinine, and urine protein levels.
- Eat a kidney-friendly diet (low sodium, moderate protein, low phosphorus and potassium)
Conclusion
Chronic kidney disease (CKD) is a lengthy journey, but there are strategies to make it less hopeless. Understanding the stages of Chronic Kidney Disease will help you manage your symptoms, protect your kidneys, and prepare for the potential need for more intensive treatment. The earlier you detect and act, the better your chances of living a whole, active life with CKD.
Frequently Asked Questions
CKD cannot be fully reversed, However, with appropriate lifestyle modifications, medicine, and illness care, its progression can be delayed or even stopped.
Absolutely. Managing blood pressure and blood sugar, avoiding NSAIDs, not smoking, and eating well can significantly slow CKD progression and improve quality of life.
If you’re at risk or have early-stages of chronic kidney disease, your doctor may recommend annual or biannual GFR and urine tests to monitor progression.
No. CKD is chronic and progressive, while acute kidney injury (AKI) is sudden and potentially reversible with prompt treatment.
Living with CKD can cause stress, anxiety, and depression, especially in later stages or when starting dialysis. Treatment must include mental health care and emotional support.