Ulcerative Colitis and Crohn’s Disease: How Do They Compare?
Inflammatory Bowel Disease (IBD) is a chronic, inflammatory condition of the gastrointestinal (GI) tract. Ulcerative Colitis and Crohn’s Disease are two of the most prevalent forms of IBD. While they have some features in common, both diseases are distinct from each other as far as diagnosis, symptoms, and treatment are concerned. Below, we introduce the most significant differences between Ulcerative Colitis and Crohn’s Disease, such as their symptoms, causes, and treatments.
What is Ulcerative Colitis?
The chronic inflammatory condition known as ulcerative colitis mostly affects the lining of the large bowel (colon) and rectum. Inflammation usually starts in the rectum and extends upward in a continuous fashion through the colon. Inflammation can form ulcers or lesions on the colon’s lining, leading to a variety of symptoms.
Symptoms of Ulcerative Colitis:
Abdominal pain and cramping – Frequently relieved after passing a bowel movement.
- Diarrhea: Often bloody or full of pus.
- Need to defecate: Sudden, urgent sensation of having to have a bowel movement.
- Fatigue: As a result of the loss of blood and inflammation.
- Weight loss: As a consequence of decreased appetite and malabsorption.
- Bleeding in the rectum: From ulcers in the lining of the colon.
- Fever: In more severe cases of inflammation.
What causes Ulcerative Colitis?
The cause of ulcerative colitis is not precisely known, but some factors are thought to predispose to it:
- Genetics: Family history comes into play, as those with a family history of having relatives with IBD are at increased risk.
- Defective immune system: A defective immune response strikes the lining of the colon.
- Environmental factors: Diet, stress, and other lifestyle factors can trigger flare-ups.
Ulcerative Colitis Treatment
The goals of treating ulcerative colitis are to reduce inflammation, manage symptoms, and bring about a permanent remission. Among the therapies are:
Medications:
- Aminosalicylates: To decrease inflammation.
- Corticosteroids: To treat short-term flare-ups.
- Immunomodulators: To dampen the abnormal immune system.
- Biologic therapies: Against specific proteins involved in inflammation.
- Surgery:
In severe cases, colectomy (removal of the colon) may be required.
What is Crohn’s Disease?
Crohn’s Disease is a form of IBD that leads to inflammation anywhere in the digestive tract, from mouth to anus. Even though Ulcerative Colitis inflames only the inner lining of the colon, Crohn’s Disease may involve deeper sections of the bowel wall. Inflammation is patchy, with normal tissue in between patches.
Symptoms of Crohn’s Disease:
- Abdominal pain and cramping : usually severe and persistent.
- Diarrhea : Occasionally with blood, depending upon where the inflammation is located.
- Fatigue : From chronic inflammation and compromised absorption of nutrients.
- Weight loss and malnutrition : From a decreased appetite and compromised absorption.
- Mouth sores : Mouth ulcers.
- Fistulas and abscesses : In rare cases, the inflammation may assume abnormal tracts or pus-filled pockets.
What Causes Crohn’s Disease?
Like Ulcerative Colitis, the etiology of Crohn’s Disease is unknown but is likely to include:
Genetics – Risk of acquiring Crohn’s Disease is higher if one has a family history.
Immune system abnormalities – The immune system attacks healthy cells in the GI tract.
Environmental – Smoking, diet, and stress can initiate or exacerbate symptoms.
Treatment of Crohn’s Disease
The goal of Crohn’s disease treatment is to reduce inflammation, minimize symptoms, and prevent complications. Among the available treatments are
Medications:
Anti-inflammatory drug: To decrease inflammation of the intestines.
Immune system suppressants : To change the immune response.
Antibiotics : To control infection and prevent fistulas.
Biologic therapies : Against proteins inducing inflammation.
Nutritional Therapy:
Specialized diet or food supplements to enhance nutrient uptake.
Surgery:
When there are complications such as fistulas, obstruction, or excessive symptoms, surgery is an option.
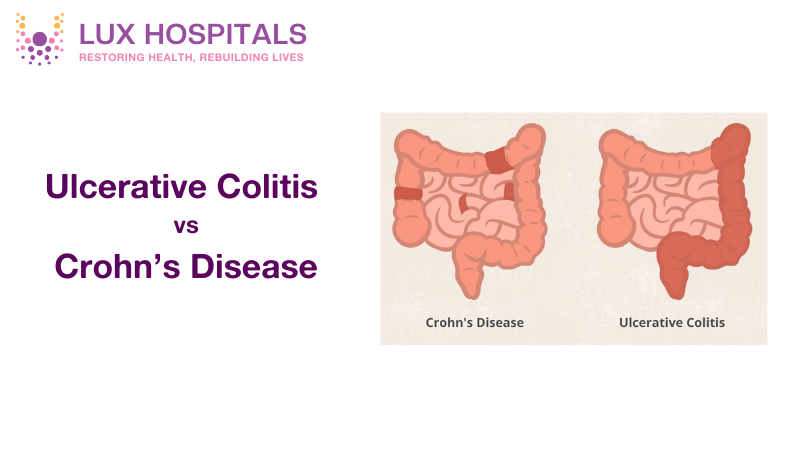
While both conditions fall under the umbrella of Inflammatory Bowel Disease, they have distinct characteristics:
| Aspect | Ulcerative Colitis | Crohn’s Disease |
| Location | Affects only the colon and rectum | Can occur anywhere along the digestive tract |
| Pattern of Inflammation | Continuous inflammation in the colon | Patchy inflammation with healthy areas between lesions |
| Depth of Inflammation | Affects only the inner lining of the colon | Can affect all layers of the bowel wall |
| Symptoms | Bloody diarrhea, abdominal pain, urgency | Abdominal pain, weight loss, diarrhea, fatigue |
| Surgical Treatment | Colectomy can cure Ulcerative Colitis | Surgery can manage symptoms but is not a cure |
Complications and Long-Term Outlook
Ulcerative Colitis and Crohn’s Disease can both develop complications if not controlled well:
Ulcerative Colitis Complications:
Colon Cancer : Elevated risk, particularly with chronic Disease.
Toxic Megacolon : Sudden distension of the colon that needs to be addressed urgently.
Liver disease : Primary sclerosing cholangitis (inflammation of the bile ducts).
Crohn’s Disease Complications:
Intestinal Obstructions : Because of narrowing or scarring.
Fistulas: Abnormal passage between segments of the bowel.
Malnutrition : Because of impaired absorption of nutrients.
Diagnosing Ulcerative Colitis and Crohn’s Disease
Accurate diagnosis is necessary for effective treatment. Tests used to diagnose are:
- Colonoscopy: Looks at the colon for ulcers and inflammation.
- Endoscopy : Looks at the upper GI tract for Crohn’s Disease.
- Biopsy: Tissue samples to differentiate between the two diseases.
- Imaging Tests : A CT scan or MRI to visualize the GI tract in detail.
- Blood Tests : To ensure anemia, inflammation, and infection.
Living With IBD
Both need lifelong treatment. Some of the strategies are outlined below:
Diet and Nutrition: Avoid trigger foods and follow a balanced diet.
Stress Management: Engage in stress-reduction methods, yoga, or mindfulness.
Adherence to Medications:
Continue your treatment and use medicine to control your symptoms.
- Regular Checkup: Follow the health of patients and adjust the treatment if needed.
- Support Groups: Meet other people suffering from the same condition to receive emotional support.
Conclusion
One should know the difference between Ulcerative Colitis and Crohn’s Disease to conduct an effective diagnosis and treatment. Although they have a similar presentation and etiology, they differ according to their location, pattern of inflammation, and treatment. In case you experience repeated gastrointestinal symptoms, seek the services of a healthcare professional for accurate diagnosis and personalized treatment.
Both diseases can affect your daily life intensely, but individuals can live a full life through appropriate treatment and lifestyle changes. If you want professional medical suggestions or high-class treatments, specialists at Lux Hospitals are available. Our professional physicians give full-care treatment and attentive care for inflammatory bowel diseases and aim to produce the best results.
Frequently Asked Questions
Remember that Ulcerative Colitis affects only the colon in a continuous pattern, while Crohn’s Disease can occur anywhere in the digestive tract in patchy areas. Think “Colon for Colitis” and “Cross for Crohn’s” (crossing the entire GI tract).
Most people with Crohn’s disease can live a normal lifespan with proper management and treatment. However, complications can impact quality of life, so regular medical care is essential.
Currently, there is no cure for either condition. However, Ulcerative Colitis can be “cured” by surgically removing the colon. Crohn’s Disease cannot be cured but can be managed with medication, lifestyle changes, and sometimes surgery to relieve symptoms and complications.
Yes, dietary changes can help manage symptoms by avoiding trigger foods such as dairy, fatty foods, and high-fiber items. Stress management techniques like mindfulness and regular exercise also help reduce flare-ups.
Genetics play a role in both conditions. Individuals with a family history of IBD are at a higher risk of developing either Ulcerative Colitis or Crohn’s Disease.
You should see a doctor if you experience persistent abdominal pain, chronic diarrhea, blood in your stool, unexplained weight loss, or severe fatigue. Prompt medical attention can help manage symptoms and prevent complications.