When Do You Need a Hysterectomy? Medical Reasons You Should Know
Hysterectomy—the surgical removal of the uterus—is one of the most common gynecologic procedures worldwide. Still, it’s not always the first or only option. Many conditions can be managed with medication, minimally invasive procedures, or watchful waiting. So, when is a Hysterectomy truly necessary? Below, you’ll find the evidence-based reasons doctors typically recommend this surgery, what each diagnosis means, alternatives you might try first, and how to make a confident, informed decision. By the end, you’ll better understand when a Hysterectomy is appropriate, what the surgery involves, and how recovery usually looks.
Medical Reasons for a Hysterectomy
There are several medical conditions where a Hysterectomy becomes the most effective or necessary treatment. These include fibroids, heavy bleeding, adenomyosis, endometriosis, uterine prolapse, cancer, chronic pelvic pain, and even rare emergencies like severe obstetric bleeding. Understanding these reasons helps patients see why doctors may recommend a Hysterectomy when other treatments fail or when it is the safest, most definitive solution.
1. Symptomatic Uterine Fibroids (When They’re Big, Multiple, or Refractory)
Noncancerous growths called fibroids might result in heavy periods. anemia, pelvic pressure, urinary frequency, constipation, and pain. Many people improve with medicines (like hormonal therapy) or procedures that shrink or remove fibroids, such as uterine artery embolization or myomectomy. Hysterectomy becomes a strong option when bleeding remains severe, fibroids rapidly regrow, fertility is no longer desired, or the uterus is so enlarged that quality of life is compromised.
2. Heavy or Abnormal Uterine Bleeding That Doesn’t Respond to Treatment
Chronic heavy menstrual bleeding can lead to iron-deficiency anemia, fatigue, and missed work. Typically, clinicians first try non-surgical options, including NSAIDs, tranexamic acid, hormonal pills, IUDs, endometrial ablation, or addressing underlying disorders like thyroid disease or coagulation issues. Suppose you’ve tried appropriate therapies and bleeding persists or recurs. In that case, a Hysterectomy may be recommended as a definitive, curative solution—especially when childbearing is complete.
3. Adenomyosis Causing Severe Pain and Bleeding
When endometrial tissue develops in the uterus, adenomyosis takes place. muscle, creating a boggy, tender uterus and painful, heavy periods. Hormonal therapies or an IUD can provide relief for many, but not all. When pain remains debilitating, periods are prolonged, and imaging plus clinical exams point to adenomyosis as the main culprit, Hysterectomy often provides lasting relief because it removes the source of the disease.
4. Endometriosis With Uterine-Dominant Disease or Coexisting Conditions
Endometriosis is driven by tissue similar to the uterine lining growing outside the uterus; surgery typically targets these implants rather than the uterus itself. However, some patients have overlapping adenomyosis or severe uterine pain/bleeding that doesn’t respond to medical suppression or conservative surgery. In those carefully selected cases—notably when fertility is not a concern—a Hysterectomy (sometimes with removal of ovaries, depending on age, symptoms, and risks) can reduce pain and bleeding that are uterine in origin.
5. Uterine Prolapse and Pelvic Organ Support Failure
When weak pelvic muscles cause the uterus to drop into the vaginal canal, symptoms can include pressure, bulge, urinary leakage, and difficulty emptying the bladder or bowels. Pelvic floor therapy, pessaries, and uterus-sparing surgeries (like hysteropexy) are valid options. Suppose prolapse is severe or recurrent, and repair goals are best met by removing the uterus. In that case, a Hysterectomy may be part of a comprehensive pelvic reconstructive procedure to restore anatomy and function.
6. Cancer or Pre-Cancer of the Uterus, Cervix, or Ovaries
For confirmed endometrial (uterine) cancer and in many cases of complex atypical hyperplasia (a pre-cancer), Hysterectomy is a cornerstone of treatment. It may also be indicated for certain cervical cancers and risk-reducing surgery in high-risk patients (for example, those with specific genetic syndromes), often combined with the removal of ovaries and fallopian tubes. In oncology settings, a Hysterectomy is not only therapeutic but also helps stage the disease and guide additional treatments.
7. Persistent, Uterine-Source Pelvic Pain After Exhausting Other Options
Chronic pelvic pain is complex and may involve the uterus, pelvic floor, bladder, bowel, nerves, or musculoskeletal sources. Before surgery, a thorough evaluation should rule out treatable conditions and consider non-surgical therapies like pelvic floor PT, neuropathic pain medications, and targeted procedures. When the pain is linked to the uterus—such as with refractory adenomyosis or severe abnormal bleeding—Hysterectomy can significantly improve quality of life.
8. Life-Threatening Obstetric Emergencies (Rare but Critical)
In uncommon situations like uncontrollable postpartum hemorrhage or placenta accreta spectrum, Hysterectomy can be lifesaving. These urgent scenarios are decided in real time by a multidisciplinary team focused on stabilizing the parent. While rare, there remain essential medical reasons where a Hysterectomy is the most effective way to stop severe bleeding.
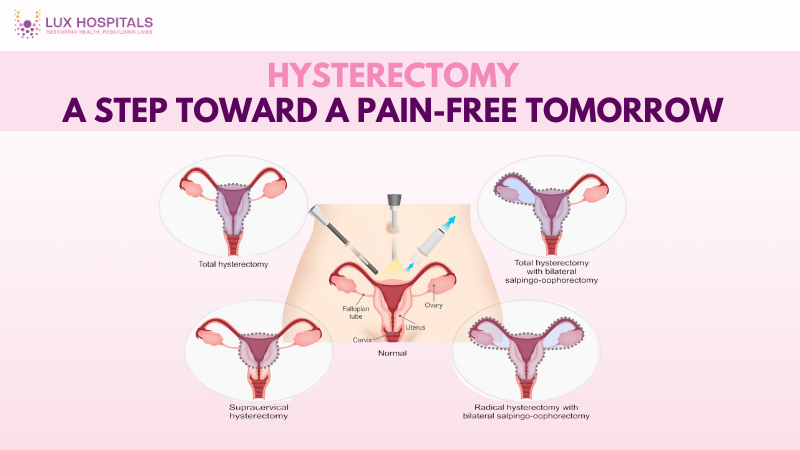
Types of Hysterectomy and How It’s Performed
The type of Hysterectomy depends on diagnosis, anatomy, and treatment goals. The uterus and cervix are removed during a hysterectomy.
- Subtotal/Supracervical Hysterectomy—removes the uterus but leaves the cervix intact.
- Minimally invasive approaches include:
- Vaginal
- Laparoscopic
- Robotic
- These often mean smaller incisions, less pain, and quicker recovery.
- Open abdominal surgery may be needed for huge fibroids, cancer staging, or complex anatomy.
The care team selects the most appropriate surgical method based on your condition.
Risks, Recovery, and What to Expect
- Risks of Hysterectomy may include:
- Bleeding
- Infection
- Blood clots
- Injury to nearby organs
- Anesthesia-related complications
- Recovery process:
- Most minimally invasive Hysterectomy patients go home the same day or after one night.
- Activity restrictions are needed for several weeks.
- Gradual return to normal daily activities is expected.
- Ovary removal considerations:
- The removal of the ovaries may result in menopausal symptoms. appear.
- If preserved, natural hormones continue, but periods stop.
- Clinicians guide whether to keep or remove ovaries and help manage hormonal changes.
Conclusion
Choosing to have a hysterectomy is a very personal decision that should be guided by a comprehensive medical evaluation and candid conversation with your physician. You can make an informed decision that feels right for you by carefully considering your fertility objectives, treatment options, diagnosis, and quality of life. When the uterus is the confirmed source of persistent symptoms, or when cancer is involved, a Hysterectomy often stands as the most reliable, long-term solution for restoring health and well-being.
Frequently Asked Questions
A total Hysterectomy removes the uterus and cervix, while a partial (supracervical) one removes the uterus but leaves the cervix in place. Your surgeon recommends one based on your diagnosis, anatomy, and cancer risk
No—ovary removal (oophorectomy) is a separate decision from Hysterectomy. In many benign cases, ovaries are preserved to maintain natural hormones, especially in younger patients. In cancer care or high-risk genetic situations, removing the ovaries may be advised to reduce recurrence or future cancer risk.
Recovery varies by surgical approach and individual health. Many people resume light activities within 2-4 weeks after a minimally invasive Hysterectomy, with full recovery often around 6 weeks. Your doctor will tailor activity restrictions and follow-up based on how you’re healing
Yes, options include medication, a hormonal IUD, uterine artery embolization, MRI-guided focused ultrasound, and myomectomy. These can reduce bleeding and pressure without removing the uterus.
If your ovaries are preserved, you won’t enter menopause immediately after a Hysterectomy, though you will stop having periods. If your ovaries are removed, menopause begins, and your team can discuss symptom management strategies.
It can, but only if the pain source is uterine. A thorough evaluation should exclude other causes like pelvic floor dysfunction, bladder pain, or nerve-related conditions before considering a Hysterectomy. When pain is uterine and other treatments fail, outcomes are often favorable.