Stages of Bladder Prolapse: From Mild to Severe
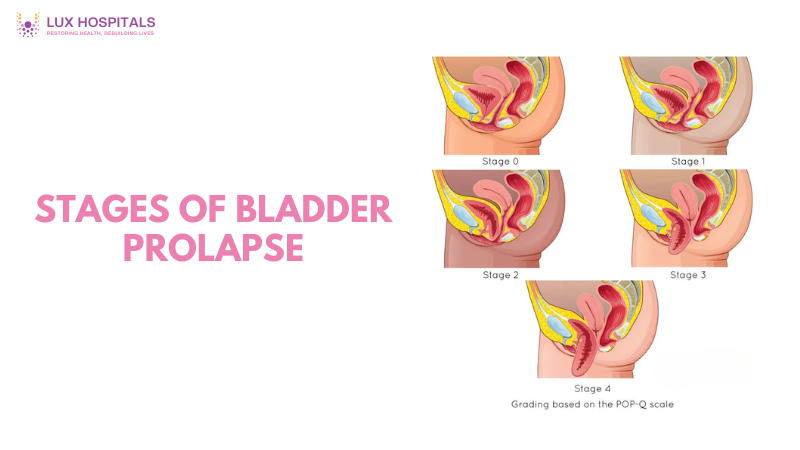
A frequent pelvic floor condition called stages of bladder prolapse, or cystocele, occurs when the bladder slides into the vaginal wall as a result of weakening muscles and tissues. Women are primarily affected by this illness, particularly following menopause or childbirth. Understanding the progression of the stages of bladder prolapse from mild to severe helps in timely diagnosis, effective management, and preventing complications.
What is bladder prolapse?
When the pelvic floor muscles weaken and are unable to support the bladder, prolapse occurs, let it fall and come into contact with the vaginal wall. The severity can range from barely noticeable discomfort to significant bulging outside the vaginal opening. Hormonal changes, ageing, childbirth, chronic constipation, and heavy lifting contribute to this condition.
Symptoms may vary by stage but can include:
- A sensation of pelvic pressure or fullness
- Urinary incontinence or retention
- Pain or discomfort during intercourse
- Visible bulging in severe cases
The stages of bladder prolapse are classified into four grades based on how far the bladder has descended.
Stages of Bladder Prolapse
Stage 1: Mild Bladder Prolapse
In stage 1 bladder prolapse, the bladder has slightly dropped but remains within the vagina. At this point, symptoms are minimal and might include occasional pelvic discomfort, a slight feeling of heaviness, or urinary urgency. Many women may not even realise they have a prolapse at this stage, as the signs are subtle and easily mistaken for general fatigue or muscle strain.
Doctors often discover Stage 1 bladder prolapse during routine pelvic exams. Treatment typically involves non-surgical interventions such as:
- Pelvic floor physical therapy
- Kegel exercises
- Lifestyle changes like avoiding heavy lifting or constipation
The condition can be kept from getting worse with early intervention.
Stage 2: Moderate Bladder Prolapse
Stage 2 bladder prolapse means the bladder has dropped further and now sits closer to the vaginal opening. Women might start to feel more pronounced symptoms such as:
- Difficulty starting or completing urination
- A frequent need to urinate
- Sensation of a bulge during physical activity or after standing for long periods
Quality of life may decline at this stage, especially if left untreated. Treatment options include vaginal pessaries, which provide structural support, and continued pelvic floor strengthening exercises. Generally speaking, surgery is not advised unless the prolapse gets worse or conservative measures are ineffective.
Stage 3: Advanced Bladder Prolapse
The bladder bulges to or through the vaginal opening in stage three bladder prolapse. Daily activities are severely hampered by this period. Typical signs and symptoms include:
- Having trouble putting tampons in
- Pain when having sex
- Leakage or retention of urine
- feeling as though “something” is dropping out of the vagina
For women with stage 3 bladder prolapse, non-surgical approaches are frequently insufficient. Urogynecologists could advise long-term pessary use or reconstructive pelvic surgery. Since problems with intimacy and body image can occur, emotional support is also crucial.
Stage 4: Severe Bladder Prolapse
Stage 4 bladder prolapse is the most advanced and visibly noticeable form, where the entire bladder has protruded outside the vaginal opening. It causes severe discomfort, pain, and significant urinary problems. Walking, sitting, or even lying down may become difficult due to the constant pressure and exposed tissue.
This stage requires surgical repair to reposition the bladder and reinforce the pelvic floor. Surgical options include native tissue repair, mesh-augmented, or minimally invasive robotic surgeries. Full recovery involves several weeks of restricted activity and physical therapy to maintain results.
Managing and Preventing Stages of Bladder Prolapse
Though the stages of bladder prolapse can progress without warning, lifestyle choices and early detection play a vital role in management. Here are prevention and management tips:
- Performing regular Kegel exercises helps build stronger muscles in the pelvis
- Maintain a healthy weight to reduce pelvic pressure
- Steer clear of straining and heavy lifting when having bowel movements
- Treat chronic cough or constipation, which increases pelvic stress
- Seek early medical evaluation for unusual pelvic symptoms
Women at higher risk, such as those post-menopause or post-childbirth, should have regular pelvic exams to monitor for signs of the stages of bladder prolapse.
Conclusion
Women who are aware of the stages of bladder prolapse are better able to identify symptoms early and seek the proper care. The illness worsens if treatment is not received, ranging from minor discomfort to severe decline. With proactive treatment ranging from pelvic exercises to surgery—women can manage or reverse symptoms.
Maintaining bladder health and preventing further difficulties from bladder prolapse requires pelvic floor support, good lifestyle choices, and routine medical examinations. It’s critical to discuss any changes in pelvic health with your healthcare physician honestly, regardless of the stage. Preserving comfort and confidence can be significantly impacted by early action.
FAQs
What are the early signs of bladder prolapse?
Early signs of bladder prolapse often go unnoticed. Women may feel a mild pressure or heaviness in the pelvis, a slight bulging sensation, or occasional urinary urgency. In some cases, mild incontinence or trouble fully emptying the bladder might occur. These symptoms are subtle but can worsen over time if left unaddressed.
How do doctors diagnose bladder prolapse?
The diagnosis of bladder prolapse begins with a pelvic examination, during which the doctor assesses the degree of bladder descent. In some cases, imaging tests like a pelvic ultrasound or MRI may be used for confirmation. Urodynamic testing helps evaluate bladder function and urinary issues. The diagnosis also includes reviewing patient history, childbirth experience, and menopause status.
Can bladder prolapse heal on its own?
Mild cases of bladder prolapse, especially Stage 1, may improve with pelvic floor exercises and lifestyle changes. However, the condition does not typically heal completely without intervention. Without proper management, it may progress to moderate or severe stages. Early detection and regular pelvic strengthening can significantly improve outcomes and may prevent surgery.
What happens if bladder prolapse is left untreated?
If bladder prolapse goes untreated, it may worsen, leading to more significant bladder descent and severe urinary dysfunction. Women may develop chronic urinary tract infections, incontinence, or sexual discomfort. Advanced stages can cause emotional distress and physical limitations. Timely treatment can prevent complications and preserve quality of life.
Is surgery always required for bladder prolapse?
Surgery is not always necessary for bladder prolapse, especially in early or moderate stages. Physical therapy, behaviour modification, and pessaries are non-surgical therapies that frequently work well. When symptoms are severe or quality of life is significantly compromised, surgery becomes a possibility. The degree of the prolapse, general health, and patient preference all influence the choice.